If you’ve ever woken up unable to lift your arm without letting out a noise that can only be described as part groan, part whale song, there’s a chance your shoulder is staging a rebellion. And sometimes that rebellion comes in the form of—wait for it—calcium crystals growing within your rotator cuff tendons.
Yes. Your shoulder can grow its own rock collection. Charming, isn’t it?
Welcome to calcific tendinopathy of the shoulder: a condition that sounds dramatic, feels dramatic, but with the right care, usually has quite a positive outcome.

What Is Calcific Tendinopathy, Really?
Calcific tendinopathy occurs when calcium deposits (usually hydroxyapatite) accumulate within the rotator cuff tendons, most commonly the supraspinatus. The condition tends to follow a predictable lifecycle, with stages ranging from silent crystal formation to an inflammatory phase that can make even the bravest patient swear that something is “very, very wrong in there.”
The process typically includes:
- A formative stage, where deposits quietly build (and patients may have zero symptoms),
- A resorptive stage, when the body decides it suddenly wants its calcium back — causing significant inflammation,
- And a post-calcific stage, where healing and tendon repair kick in.
Most patients start seeking help during the “why does this hurt so much?” phase — also known scientifically as the resorptive stage.
What Does It Feel Like?
The hallmark of calcific tendinopathy is shoulder pain, often intense, sometimes unprovoked, and occasionally dramatic enough to send people Googling phrases like “is my arm falling off?”
Symptoms often include:
- Sharp or aching pain in the front or outer shoulder
- Pain that worsens with overhead movements
- Night pain (because of course it waits for bedtime)
- Limited range of motion
- A feeling of “catching” or stiffness
- Weakness in the rotator cuff due to pain inhibition
During the resorptive phase, symptoms can mimic rotator cuff tears or frozen shoulder in severity — but take heart: this is often when the deposit is preparing to break down.
How Is Calcific Tendinopathy Diagnosed?
A good clinical examination will usually reveal pain with resisted abduction or flexion, difficulty lifting the arm, and local tenderness over the rotator cuff. But because many shoulder pathologies enjoy blending together like a surprise smoothie, imaging is the real MVP here.
Ultrasound is typically the gold standard due to its ability to visualise deposits clearly and guide treatment.
X-ray can also reveal calcium densities, especially in larger deposits.
MRI is rarely needed unless other pathology is suspected (e.g., full-thickness tears).
As chiropractors, we collaborate closely with imaging centres when needed to make sure you’re getting an accurate diagnosis and an efficient care pathway.
…But What Else Could It Be?
Shoulder pain is a shapeshifter. Before declaring “calcium crystals did it!”, we consider:
- Rotator cuff tendinopathy/tear — similar movement pain but no calcifications on imaging.
- Subacromial impingement — typically activity-related and improves with postural or mechanical correction.
- Adhesive capsulitis — significant global stiffness; usually a slower onset compared with the often acute flare of calcific tendinopathy.
- Acromioclavicular joint pathology — very localised pain at the top of the shoulder.
- Cervical radiculopathy — neck involvement, neurological signs, and pain referring down the arm rather than just the shoulder.
A key differentiator is night pain combined with severe, sometimes unprovoked flare-ups — a classic hint that a deposit is actively resorbing.
How Chiropractors Help: Treatment That Doesn’t Involve a Chisel
Good news: no one is mining your shoulder. Conservative care is highly effective, and chiropractors are well-placed to guide both acute management and rehabilitation.
Treatment focuses on reducing pain, restoring movement, and optimising the mechanics of the shoulder so the tendon can heal without unnecessary strain.
Care options typically include:

Manual Therapy & Joint Mobilisation
Gentle mobilisations help improve joint mechanics, reduce guarding, and restore range of motion. Soft-tissue work around the rotator cuff, biceps tendon, and upper back helps decrease secondary tension.
Needling Options
Dry needling may help reduce muscular guarding (not the deposit itself), improving comfort and range.
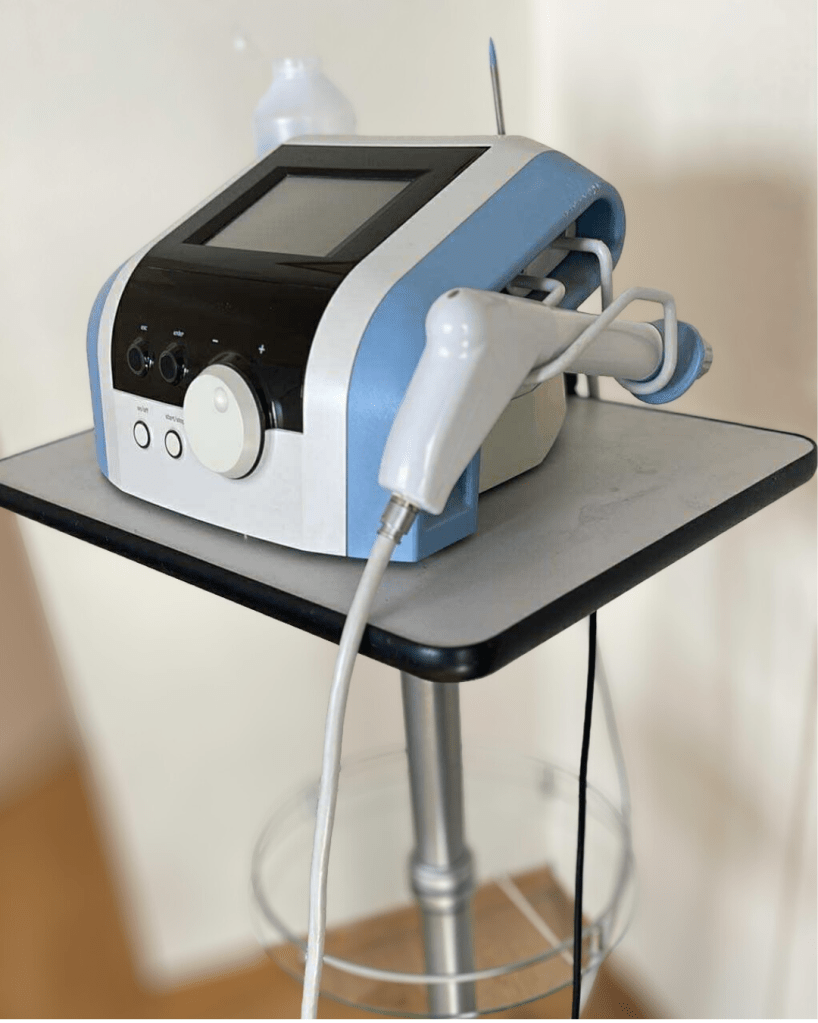
Shockwave Therapy (ESWT)
One of the most evidence-supported treatments for calcific tendinopathy, especially in the resorptive and early rehabilitation phases. Shockwave can help break down deposits, reduce pain, and speed up recovery by stimulating local biological healing.
Exercise Rehab
Targeted rehab focuses on:
- restoring pain-free movement,
- re-training scapular mechanics,
- strengthening the rotator cuff and surrounding stabilisers,
- progressing to functional and sport-specific loading.
Exercise remains one of the most effective long-term strategies — especially after the deposit has broken down.
When We Refer Out (The “Red Flag” Section)
Although calcific tendinopathy is usually benign, some situations warrant further medical input:
- Suspicion of infection, fracture, or systemic inflammatory condition
- Severe, escalating pain unresponsive to conservative care
- Neurological deficits
- A failure to improve over several weeks despite appropriate management
For very stubborn cases, options like ultrasound-guided barbotage (a lavage technique to break up and aspirate the deposit) or cortisone injections may be used. And only in rare, severe, and persistent cases is surgery considered.
After the Storm: Rehab & Long-Term Care
Once the flare settles, rehab becomes the hero of the story. The goal isn’t just to banish the pain — it’s to prevent your shoulder from re-enacting the calcium-collecting hobby it has so enthusiastically adopted.
Rehab focuses on restoring full range of motion, healthy tendon loading, postural strength, and balanced scapular control. Follow-up care may include periodic check-ins, progressive strengthening, and ergonomic advice for work, sport, and day-to-day movement patterns.
And good news: once resolved, calcific tendinopathy rarely returns with the same vengeance!
References
Cho, N. S., Lee, B. G., Rhee, Y. G. (2015). Radiologic and clinical outcomes after treatment of chronic calcific tendinitis with ultrasound-guided needling. American Journal of Sports Medicine.
Del Castillo-González, F., et al. (2016). Effectiveness of extracorporeal shockwave therapy in calcific tendinopathy of the shoulder. Journal of Orthopaedics & Traumatology.
Harvie, P., et al. (2017). Calcific tendinopathy of the rotator cuff: Natural history and association with endocrine disorders. Journal of Shoulder and Elbow Surgery.
Louwerens, J. K., et al. (2014). The reliability of the diagnosis of subacromial impingement syndrome and rotator cuff tendinopathy. Musculoskeletal Science & Practice.
Sansone, V., & Maiorano, E. (2013). Calcific tendinopathy: A review. Journal of Sports Medicine and Physical Fitness.
Speed, C. (2014). Shockwave therapy in musculoskeletal disorders. BMJ.
Uhthoff, H., & Loehr, J. (2014). Calcific tendinopathy of the rotator cuff: Pathogenesis, diagnosis, and management. Journal of the American Academy of Orthopaedic Surgeons.





Leave a comment